Blog

Reasons for Corns

A corn that develops on the foot can produce severe pain and discomfort. It happens as a result of excessive pressure that is put on a specific part of the foot from the worn shoes. The places where corns can develop are on the side of the pinky toe, the soles of the feet, or on top of the toes. Many people choose to wear shoes that are too tight because of workplace policies or for appearance reasons, and this may be why corns can develop. Patients who have corns that are not treated or removed may notice their gait or walking style is compromised, which is a defense mechanism against the pain. Mild relief may be found when the foot is soaked in warm water, and a pumice stone is used which may reduce the size of the corn. This is generally a temporary fix and the corn may reappear if not treated permanently. If you are afflicted with a corn, it is strongly suggested that you speak to a podiatrist who can offer you several treatment options.
If you have any concerns regarding your feet and ankles, contact Queen Mbanuzue, DPM of In Step Podiatry Center. Our doctor will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctor to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Lanham, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Corns
Corns are hard and thick areas of skin that form as a result of constant rubbing, friction, or pressure on the skin. They are patches of dead skin with a small plug toward the center. They may appear on the tops and sides of toes and can make walking painful.
Soft corns are typically thinner with a white color and rubbery texture. Soft corns tend to appear between the toes. Seed corns are another type of corn that appear in clusters and can be tender if they are on a weight-bearing part of the foot. Seed corns usually appear on the bottom of the foot and are likely caused by a blockage in sweat ducts.
While corns and calluses are somewhat similar, calluses are a bit different. Calluses are a patch of dead skin that can occur anywhere on the body. In comparison to corns, calluses are usually a bit larger in size. However, both corns and calluses are caused by increased friction on the skin.
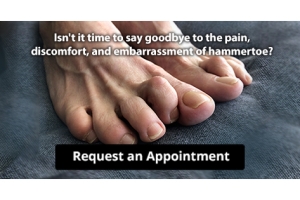
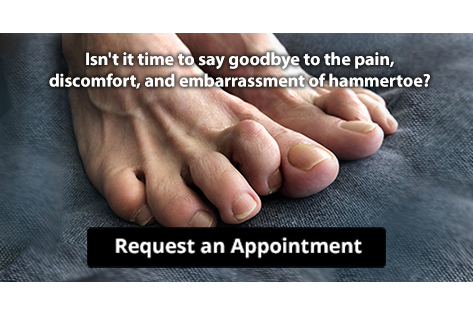
There are some risk factors that may increase your chances of developing corns and calluses. If you have bunions, hammertoe, or a bone spur, you are more likely to develop a corn or callus on your foot.
While Corns and Calluses tend to disappear when the friction to the affected area ceases, the help of a podiatrist may be useful in the removal process. It is important to remove the dead skin around the area and this may be done in a few different ways. Moisturizing creams may be helpful in softening and removing the dead skin around the callus. You should never use razors or other pedicure equipment to remove your corns. Doing this may worsen your corn or callus and cause infection.
In some cases, corns and calluses may be caused by abnormal foot structure or walking motion. In such a case, you should seek a podiatrist’s assistance in order to correct the issue.
What Causes Plantar Fasciitis?

The foot condition referred to as plantar fasciitis can cause severe heel pain. It affects the plantar fascia, which is the band of tissue that connects the heel to the toes, and is located on the sole of the foot. Repetitive running and overuse may cause the plantar fascia to become inflamed or torn, and this often requires medical attention. Many patients notice the pain is worse in the morning after arising, and may become milder as the foot warms up while walking. This condition may occur from standing on hard or uneven surfaces for most of the day, or possibly from wearing shoes that have little or no support. Mild relief may be found when custom-made orthotics are worn, and this may help to take pressure off of the plantar fascia. If you have heel pain, it is strongly advised that you are under the care of a podiatrist who can effectively diagnose and properly treat plantar fasciitis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Queen Mbanuzue, DPM from In Step Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Lanham, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Fissures Are Severely Cracked Heels

Mild cases of cracked heels generally are not concerning, and a good moisturizer may be used to help control this condition. Severe cracks in the skin are referred to as fissures and can bleed and cause pain. They can develop as a result of standing on hard surfaces for most of the day, or from wearing shoes that have an open back. There may be existing medical conditions that can lead to getting cracked heels. These can consist of different types of dermatosis, psoriasis, and thyroid disorders. Additionally, people who are obese may experience cracked heels, which may come from the extra weight the heels endure while standing and walking. The most effective way of treating cracked heels is by preventing them from happening. This can be done by drinking plenty of water daily, and frequently applying a good moisturizer on them. Some people enjoy using a pumice stone on their heels to remove dead skin that may have developed. If you have cracked heels, it is urged that you consult with a podiatrist who can guide you toward the correct treatment methods, which may include prescribing medication.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Queen Mbanuzue, DPM from In Step Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Lanham, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Facts About Plantar Warts

A plantar wart, also called a verruca, is believed to be caused by the human papillomavirus (HPV) and results in the buildup of keratin on the skin. This shows up as a wart. Because HPV thrives in warm, moist environments, it may be spread by walking barefoot around swimming pools or gym locker rooms. It frequently enters through a crack or sore on the bottom of the foot. Plantar warts often cause pain, which can be felt when putting weight on the foot. Other symptoms include thickened skin that appears to be a callus and black dots, which are actually dried blood trapped in the capillaries. Sometimes, white or skin-colored lesions appear on the sole of the foot. Plantar warts often go away on their own, but the foot may be re-exposed if proper footwear is not used in situations where HPV is likely to be found. A podiatrist can offer a number of treatment options to remove a plantar wart. Among them are burning off the wart with salicylic acid, freezing the wart, or cutting the wart out. For more information, please consult a podiatrist.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Queen Mbanuzue, DPM from In Step Podiatry Center. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Lanham, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
All About Plantar Warts
Plantar warts are warts that are only found on the feet, hence the term “plantar”, which means “relating to the foot.” They are caused by the human papillomavirus, or HPV, and occur when this virus gets into open wounds on the feet. The warts themselves are hard bumps on the foot. They are easily recognizable, mostly found on the heels or ball of the foot. Plantar warts are non-malignant, but they can cause some pain, discomfort, and are often unsightly. Removing them is a common step toward treating them.
Plantar warts can cause some pain while standing, sometimes felt as tenderness on the sole of your foot. Unless the wart has grown into the foot behind a callus, you will be able to see the fleshy wart. A podiatrist should only be consulted if there is an excessive amount of pain. Plantar warts are not cancerous or dangerous, but they can affect your walking and continually reappear. Anyone who suffers from diabetes or a compromised immune system disease should seek out care immediately.
Podiatrists are easily able to diagnose plantar warts. They usually scrape off a tiny bit of the rough skin to make tiny blood clots visible and examine the inside of warts. However, a biopsy can be done if the doctor is not able to diagnose them from simply looking at them. Although plantar warts usually do not require an excessive amount of treatment, there are ways to go about removing them. A common method is to freeze them off using liquid nitrogen, removing them using an electrical tool, or burning them off via laser treatment. For a less invasive treatment option, topical creams can be used through a doctor’s prescription. This treatment method takes more time, however. Keep the wart covered for protection in between daily treatments.
The best way to avoid developing plantar warts is to avoid walking barefoot in public places. Avoid this especially if you have open sores or cuts on your feet. It is also important to avoid direct contact with warts in general, as they are highly contagious.
Mandatory Education for Podiatrists

People who experience painful or uncomfortable conditions regarding the foot and ankle often seek the advice of a podiatrist. These are doctors that specialize in treating a multitude of disorders concerning the feet. They are trained in diagnosing and treating foot conditions. The extensive schooling that is needed to pursue this type of career consists of obtaining a bachelor’s degree, followed by completing a Doctor of Podiatric Medicine program. This typically takes approximately four years to finish, and then a residency will take place in a hospital for three years. There are tests that must be passed to be licensed in a particular state to practice in. When the above tasks are completed, a podiatrist can choose what type of places to work in. These can consist of hospitals, private or group practices, in addition to extended care facilities. If you are considering pursuing a career in podiatry, it is strongly suggested that you speak with this type of doctor who can help you in determining if this is a right choice for you.
If you are experiencing pain in the feet or ankles, don’t join the stubborn majority refusing treatment. Feel free to contact Queen Mbanuzue, DPM from In Step Podiatry Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
Someone would seek the care of a podiatrist if they have suffered a foot injury or have common foot ailments such as heal spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, etc.
Podiatric Treatment
A podiatrist will treat the problematic areas of the feet, ankle or lower leg by prescribing the following:
- Physical therapy
- Drugs
- Orthotic inserts or soles
- Surgery on lower extremity fractures
A common podiatric procedure a podiatrist will use is a scanner or force plate which will allow the podiatrist to know the designs of orthotics. Patients are then told to follow a series of tasks to complete the treatment. The computer will scan the foot a see which areas show weight distribution and pressure points. The podiatrist will read the analysis and then determine which treatment plans are available.
If you have any questions please feel free to contact our office located in Lanham, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022